Lice Infestation (Pediculosis)
What is Lice Infestation?
Lice infestation is a condition where tiny insects called lice live on the skin, hair, or clothing of a person and feed on their blood. Lice can cause itching, irritation, and sometimes infections. Lice can be spread by close contact with an infested person or by sharing personal items such as hats, combs, or towels. There are different types of lice that affect different parts of the body, such as head lice, body lice, and pubic lice.
What are the signs and symptoms of Lice Infestation?
Some of the signs and symptoms of lice infestation are:
- Intense itching on the scalp, body or in the genital area. This is an allergic reaction to louse bites.
- A tickling feeling from movement of hair. This is caused by the lice crawling on the skin or hair.
- The presence of lice on the scalp, body, clothing, or pubic or other body hair. Adult lice may be about the size of a sesame seed or slightly larger. They are tan or grayish in color and avoid light.
- Lice eggs (nits) on hair shafts. Nits are tiny, oval-shaped eggs that stick to hair shafts near the scalp. They may be white, yellow, or brown in color and may look like dandruff, but they cannot be easily brushed out of hair.
- Sores on the scalp, neck and shoulders. Scratching can lead to small red bumps that may sometimes get infected with bacteria.
- Bite marks, especially around the waist, groin, upper thighs and pubic area. These are caused by the lice feeding on blood from the skin.
What treatments are available at the dermatologist for Lice Infestation?
Some of the treatments that are available at the dermatologist for lice infestation are:
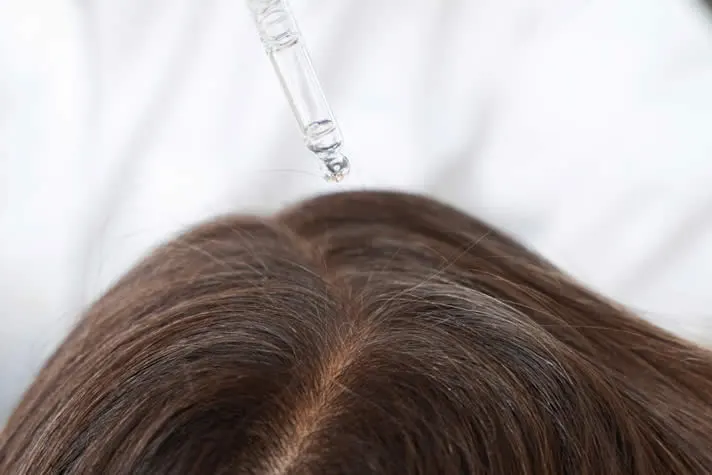
- Prescription shampoos or lotions that contain different ingredients than the over-the-counter products. These may include malathion, benzyl alcohol, or spinosad. These products are applied to the hair and scalp and left for a certain amount of time before rinsing. They may be more effective against lice that are resistant to other treatments.
- Oral prescription drug such as ivermectin. This is a tablet that is taken by mouth and kills lice by affecting their nervous system. It is usually given in two doses, eight days apart. This drug is typically used when other treatments have not been effective or when there is a widespread infestation.
- Manual removal of lice and nits. This involves using a fine-tooth comb or a special device to comb through the hair and remove the lice and their eggs. This method can be time-consuming and tedious, but it can be done at home or with the help of a professional. Manual removal may be necessary in addition to other treatments, especially for pubic lice or eyelash lice.

FAQ About Lice Infestation
How is lice infestation diagnosed?
Lice infestation is diagnosed by examining the hair and scalp for nits, nymphs (immature lice), or adult lice. A fine-toothed comb or a special device may be used to comb through the hair and remove the lice and nits. A magnifying glass or a microscope may be needed to see the lice or nits clearly. Sometimes, a skin scraping or a hair sample may be taken and sent to a laboratory for confirmation.
Is lice infestation a sign of poor hygiene or an unclean environment?
-
No. Lice infestation is not a sign of poor hygiene or an unclean environment. Anyone can get lice regardless of their personal cleanliness or living conditions. Lice are not attracted to dirt or grease, but to human blood. Lice can infest people of any age, gender, race, or socioeconomic status.
Can lice infestation affect other animals or pets?
No. Lice are species-specific, meaning they only infest humans and do not affect other animals or pets. Lice cannot be transmitted from animals to humans or vice versa.
Can lice infestation be cured?
Is there a dermatologist near me in Chula Vista that offers treatment for Lice Infestation?
Yes. At our Chula Vista dermatology office we offer treatment for Lice Infestation to patients from Chula Vista and the surrounding area. Contact our office today to schedule an appointment.




